A group of researchers at Louisiana Tech University in the United States have developed an innovative method of using a home 3D printer to manufacture customized medical implants containing drugs that are gradually released into the body, including chemotherapeutic treatments.
Until now, medical implants that release medication in a controlled manner were made in a generic way, attending to the most common doses and pathologies, not allowing individualized use with the appropriate components and doses for each patient.
Researchers at Louisiana Tech University have broken this impediment by working on a project that has developed an extruder to create a filament for medical use that can be used in home-type 3D printers. The key is in the filament, which is made with the medical compounds needed for drug release once implanted in the body, usually itradermally.
The base material of the filament is absorbed by the human body in a natural way, and it is loaded with antibiotics or other medical compounds. This makes it possible to create customized implants for each patient, adding the appropriate doses of the medications they need.
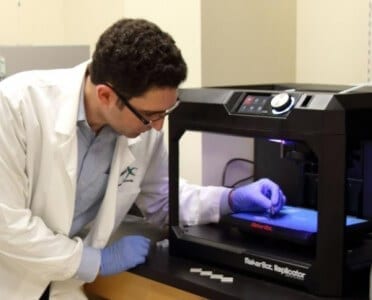
According to Jeffrey Weisman, one of the developers of the project, the use of implants for personalized drug delivery is a growing trend in the medical sector. The method of creating clinical-use filament for 3D printers will allow hospitals and pharmacies a new way to prescribe drugs. “One of the biggest benefits of this method is that we can use any home-type 3D printer that we can find anywhere in the world,” commented the researcher. In fact, the printer they have used is a MakerBot Replicator, the most widespread model of domestic 3D printers.

The system has been developed in a collaboration between departments of biomedical engineering, nanosystems and nanoelectrical systems, following an inquiry from Dr. David Mills as to whether antibiotic capsules could be 3D printed with some kind of material absorbable by the human body.
Most of today’s antibiotic implants such as discs are made of bone cement, a material that must be mixed by hand during a small surgery. These discs are usually made of plexiglass, which means they have to be removed after treatment is complete. The filament they have developed in Louisiana is a bioplastic that is absorbed into the human body avoiding this second intervention to remove the implant.
In addition, the system they have developed allows the creation of these implants with hollow areas, to allow a larger surface area in contact with the tissue and permit a more controlled release of the medication. On the other hand, the research team points out that these implants can be localized in specific areas, thus avoiding the dispersion of the drug and possible damage to other organs such as the liver or kidneys.
“Currently, incorporating the additives into the plastic requires an industrial-type facility to allow for proper dispersion throughout the plastic,” says Mills, “Our method allows for much smaller scale dispersion, making available to researchers a way to customize the additives to the levels required. There is no other process, even industrial, for making antibiotic- or drug-specific release implants, as injection molding is currently focused more on colorants and aesthetic properties,” says the researcher. “It is really novel and the first time in the world that a customized antibiotic or chemotherapy substance release device is 3D printed.”